Advancements in Prenatal Genetic Testing: A Comprehensive Guide for OB-GYN Clinicians
Introduction
Prenatal genetic testing has come a long way in recent years, offering expectant parents and healthcare providers valuable insights into the health and well-being of the developing fetus. As an OB-GYN clinician, it is crucial to stay up-to-date with the latest advancements in this field to provide the best possible care for your patients. In this comprehensive guide, we will explore the various types of prenatal genetic testing available today and discuss their benefits, limitations, and ethical considerations.
Non-Invasive Prenatal Testing (NIPT)
Non-invasive prenatal testing, also known as NIPT, has revolutionized the way we screen for chromosomal abnormalities such as Down syndrome, trisomy 18, and trisomy 13. Unlike traditional methods that carry a small risk of miscarriage, NIPT involves a simple blood draw from the expectant mother, making it a safer and more accessible option.
NIPT analyzes cell-free fetal DNA present in the mother’s bloodstream to detect the presence of extra or missing chromosomes. The results are highly accurate, with a detection rate of over 99% for common chromosomal abnormalities. However, it is important to note that NIPT is a screening test and should be followed up with diagnostic testing for confirmation.
Traditional Screening vs. NIPT
Feature | Traditional Screening (First/Second Trimester) | Non-Invasive Prenatal Testing (NIPT) |
Procedure Type | Blood test + ultrasound (nuchal translucency, serum markers) | Simple maternal blood draw |
Accuracy | ~80–90% for common trisomies (varies by test) | >99% for Down syndrome, trisomy 18 & 13 |
Risk Level | No risk to fetus, but may lead to more invasive follow-ups | No risk to fetus |
Timing | 11–14 weeks (first trimester), 15–20 weeks (second trimester) | As early as 10 weeks |
False Positive Rate | Higher (~5%) | Very low (<1%) |
Cost & Availability | Widely available, usually covered by insurance | Higher cost, coverage varies but expanding |
Diagnostic Testing
If NIPT results indicate a high risk for a chromosomal abnormality, diagnostic testing is recommended to confirm the findings. Two common diagnostic tests are chorionic villus sampling (CVS) and amniocentesis.
CVS involves the removal of a small sample of placental tissue for analysis. It is typically performed between 10 and 13 weeks of pregnancy and provides definitive results. However, there is a slightly higher risk of miscarriage compared to amniocentesis.
Amniocentesis, on the other hand, involves the extraction of amniotic fluid and is usually performed between 15 and 20 weeks of pregnancy. It carries a lower risk of miscarriage but may take longer to obtain results. Both CVS and amniocentesis can detect chromosomal abnormalities as well as other genetic conditions.
Expanded Carrier Screening
Expanded carrier screening is a type of genetic testing that assesses an individual’s risk of passing on certain genetic disorders to their offspring. Traditionally, carrier screening was limited to a few common conditions, such as cystic fibrosis and sickle cell anemia. However, advancements in technology have made it possible to screen for hundreds of genetic disorders simultaneously.
This type of testing is particularly important for couples with a family history of genetic disorders or those from certain ethnic backgrounds with a higher prevalence of specific conditions. Identifying carriers allows for informed family planning decisions and, in some cases, the option of preimplantation genetic testing during in vitro fertilization.
Microarray Analysis
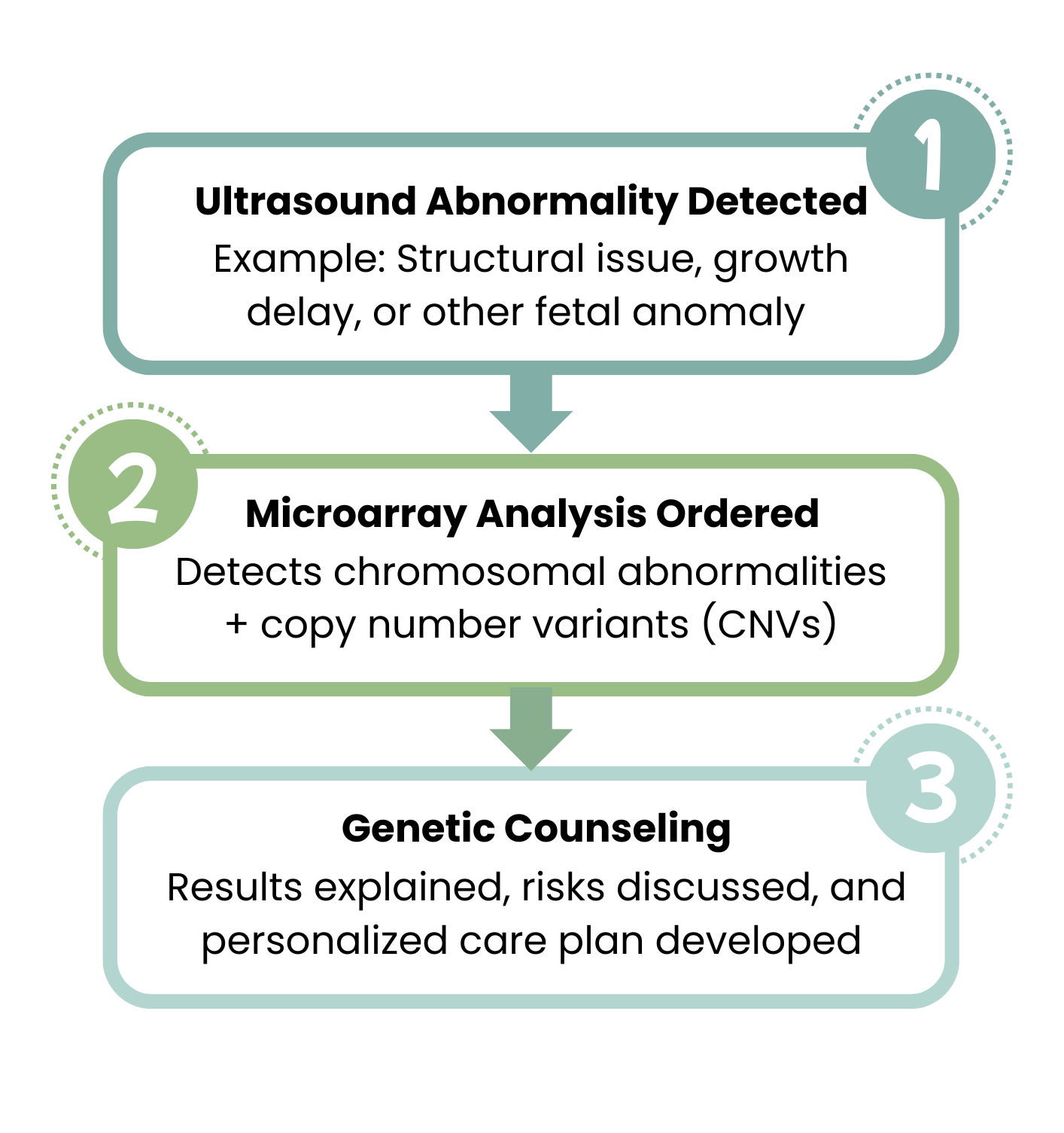
Microarray analysis is a comprehensive genetic test that can detect both chromosomal abnormalities and smaller genetic changes known as copy number variants (CNVs). CNVs are alterations in the number of copies of a particular DNA segment and can be associated with developmental delays, intellectual disabilities, and other health conditions.
This type of testing is typically recommended when there are structural abnormalities detected during an ultrasound or when there is a suspicion of a genetic condition based on the family history. Microarray analysis can provide valuable information about the genetic makeup of the fetus and guide further management and counseling.
When to Consider Microarray Analysis
Ethical Considerations
As with any medical intervention, prenatal genetic testing raises ethical considerations that must be carefully addressed. These include issues such as informed consent, privacy and confidentiality of genetic information, the potential psychological impact on expectant parents, and the possibility of selective abortion based on test results.
It is essential for OB-GYN clinicians to engage in open and honest discussions with their patients, providing them with accurate information about the benefits, limitations, and potential risks of prenatal genetic testing. Genetic counseling should be offered to help expectant parents make informed decisions and navigate the complexities associated with the results.
Conclusion
Prenatal genetic testing has become an invaluable tool in the field of obstetrics, allowing healthcare providers to offer personalized care and support to expectant parents. By staying informed about the latest advancements in this rapidly evolving field, OB-GYN clinicians can ensure that their patients receive the highest standard of care throughout their pregnancy journey.
Remember, prenatal genetic testing is just one piece of the puzzle. It should always be accompanied by comprehensive prenatal care, including regular check-ups, ultrasounds, and other necessary screenings. Together, these tools empower clinicians to provide the best possible care for both the mother and the developing fetus.
FAQ
1. Is NIPT covered by insurance?
Coverage depends on the patient’s insurance plan and risk factors. Many insurers cover NIPT for women over age 35 or those with high-risk pregnancies, but policies vary. Always verify coverage before testing.
2. When should I recommend carrier screening?
Carrier screening is best recommended before conception or early in pregnancy. It is particularly important for couples with a family history of genetic disorders or from ethnic groups with higher prevalence of certain conditions.
3. How accurate is NIPT compared to traditional screening?
NIPT has a detection rate of over 99% for common chromosomal abnormalities, far higher than traditional first-trimester screening. However, it is still a screening test and requires confirmatory diagnostic testing.
4. Does diagnostic testing like CVS or amniocentesis always carry risk?
Yes, both procedures carry a small risk of miscarriage. The risk is slightly higher with CVS than with amniocentesis, but both are considered safe when performed by experienced providers.
5. Can prenatal genetic testing detect all genetic conditions?
No. While testing methods like NIPT, carrier screening, and microarray analysis provide valuable information, they cannot identify all possible genetic conditions or birth defects.
6. How should I counsel patients who feel overwhelmed by test results?
Genetic counseling is key. Encourage patients to meet with a genetic counselor who can explain results in detail, discuss options, and provide emotional support.
7. What are the ethical concerns I should discuss with patients?
Concerns include informed consent, confidentiality of genetic information, emotional impact of results, and potential choices regarding pregnancy management. It’s critical to approach these conversations with sensitivity and transparency.





